Flatfoot
What is Flatfoot?
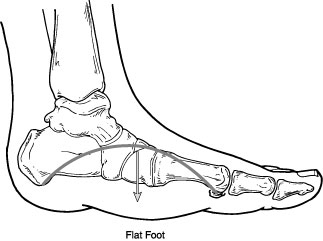
Flatfoot is often a complex disorder, with diverse symptoms and varying degrees of deformity and disability. There are several types of flatfoot, all of which have one characteristic in common—partial or total collapse (loss) of the medial longitudinal arch associated with hyperpronation.
Other characteristics shared by most types of flatfoot include:
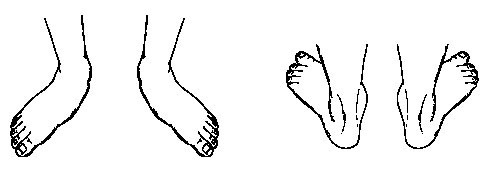
"Toe drift," where the toes and front part of the foot point outward.
The heel tilts toward the outside and the ankle appears to turn in.
A short Achilles tendon, which causes the heel to lift off the ground earlier when walking and may act as a deforming force.
Bunions and hammertoes may occur in some people with flatfeet.
Health problems such as rheumatoid arthritis or diabetes sometimes increase the risk of developing flatfoot. In addition, adults who are overweight frequently have flatfoot.
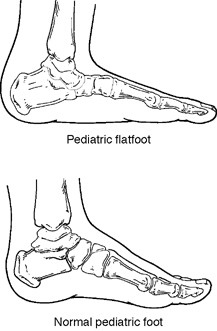
Paediatric Flatfoot
What is Paediatric Flatfoot?
What is Flatfoot?
Flatfoot is often a complex disorder, with diverse symptoms and varying degrees of deformity and disability. There are several types of flatfoot, all of which have one characteristic in common—partial or total collapse (loss) of the medial longitudinal arch associated with hyperpronation.
Other characteristics shared by most types of flatfoot include:
"Toe drift," where the toes and front part of the foot point outward.
The heel tilts toward the outside and the ankle appears to turn in.
A short Achilles tendon, which causes the heel to lift off the ground earlier when walking and may act as a deforming force.
Bunions and hammertoes may occur in some people with flatfeet.
Health problems such as rheumatoid arthritis or diabetes sometimes increase the risk of developing flatfoot. In addition, adults who are overweight frequently have flatfoot.
Paediatric Flatfoot
What is Paediatric Flatfoot?
Flatfoot
is common in both children and adults. When this deformity occurs in
children, it is referred to as “paediatric flatfoot,” a term that
actually includes several types of flatfoot. Although there are
differences between the various forms of flatfoot, they all share one
characteristic—partial or total collapse of the arch.
Most children with flatfoot have no symptoms, but some children have one or more symptoms. When symptoms do occur, they vary according to the type of flatfoot. Some signs and symptoms may include:
Pain, tenderness, or cramping in the foot, leg, and knee
Outward tilting of the heel
Most children with flatfoot have no symptoms, but some children have one or more symptoms. When symptoms do occur, they vary according to the type of flatfoot. Some signs and symptoms may include:
Pain, tenderness, or cramping in the foot, leg, and knee
Outward tilting of the heel
- Awkwardness or changes in walking
- Difficulty with shoes
- Reduced energy when participating in physical activities
- Voluntary withdrawal from physical activities
Flatfoot can be apparent at birth or it may not show up until years later, depending on the type of
flatfoot. Some forms of flatfoot occur in one foot only,
while others may affect both feet.
Types of Pediatric Flatfoot
Various terms are used to describe the different types of flatfoot. For example, flatfoot is either asymptomatic (without symptoms) or symptomatic (with symptoms). As mentioned earlier, the majority of children with flatfoot have an asymptomatic condition.
flatfoot. Some forms of flatfoot occur in one foot only,
while others may affect both feet.
Types of Pediatric Flatfoot
Various terms are used to describe the different types of flatfoot. For example, flatfoot is either asymptomatic (without symptoms) or symptomatic (with symptoms). As mentioned earlier, the majority of children with flatfoot have an asymptomatic condition.
Symptomatic
flatfoot is further described as being either flexible or rigid.
“Flexible“ means that the foot is flat when standing (weight-bearing),
but the arch returns when not standing. “Rigid” means the arch is
always stiff and flat, whether standing on the foot or not.
Several types of flatfoot are categorized as rigid. The most common are:
Several types of flatfoot are categorized as rigid. The most common are:
- Tarsal coalition . This is a congenital (existing at birth) condition. It involves an abnormal joining of two or more bones in the foot. Tarsal coalition may or may not produce pain. When pain does occur, it usually starts in preadolescence or adolescence.
- Congenital vertical talus. Because of the foot’s rigid “rocker bottom” appearance that occurs with congenital vertical talus, this condition is apparent in the newborn. Symptoms begin at walking age, since it is difficult for the child to bear weight and wear shoes
There are other types of paediatric flatfoot, such as those caused by injury or some diseases.
Diagnosis
In diagnosing flatfoot, the foot is examined and observed with the child standing and sitting. The surgeon also observes how the child walks and evaluates the range of motion of the foot. Because flatfoot is sometimes related to problems in the leg, the surgeon may also examine the knee and hip.
X-rays are often taken to determine the severity of the deformity. Sometimes an MRI study, CT scan, and blood tests are ordered.
Treatment: Non-surgical Approaches
If a child’s flatfoot is asymptomatic, traditional treatments have tended to avoid intervention with instead, the condition being observed and re-evaluated periodically. Custom orthotic devices may be considered for some cases of asymptomatic flatfoot however we now advocate use of the HyProCure sinus tarsi implant for both the asymptomatic and symptomatic flexible paediatric flatfoot.
In the symptomatic pediatric flatfoot, treatment is required and may include one or more approaches, depending on the child’s particular case.
Some examples of non-surgical options include:
Diagnosis
In diagnosing flatfoot, the foot is examined and observed with the child standing and sitting. The surgeon also observes how the child walks and evaluates the range of motion of the foot. Because flatfoot is sometimes related to problems in the leg, the surgeon may also examine the knee and hip.
X-rays are often taken to determine the severity of the deformity. Sometimes an MRI study, CT scan, and blood tests are ordered.
Treatment: Non-surgical Approaches
If a child’s flatfoot is asymptomatic, traditional treatments have tended to avoid intervention with instead, the condition being observed and re-evaluated periodically. Custom orthotic devices may be considered for some cases of asymptomatic flatfoot however we now advocate use of the HyProCure sinus tarsi implant for both the asymptomatic and symptomatic flexible paediatric flatfoot.
In the symptomatic pediatric flatfoot, treatment is required and may include one or more approaches, depending on the child’s particular case.
Some examples of non-surgical options include:
- Activity modifications. The child needs to temporarily decrease activities that bring pain as well as avoid prolonged walking or standing.
- Orthotic devices. The foot and ankle surgeon can provide custom orthotic devices that fit inside the shoe to support the structure of the foot and improve function.
- Physical therapy. Stretching exercises, supervised by the foot and ankle surgeon or a physical therapist, provide relief in some cases of flatfoot.
Medications.
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may
be recommended to help reduce pain and inflammation.
Shoe modifications. The foot and ankle surgeon will advise you on footwear characteristics that are important for the child with flatfoot.
When is Surgery Needed?
In some cases, surgery is necessary to relieve the symptoms and improve foot function. Foot and ankle sugeons perform a variety of techniques to treat the different types of pediatric flatfoot. The surgical procedure or combination of procedures selected for your child will depend on his or her particular type of flatfoot and degree of deformity.
Adult Flexible Flatfoot
Flexible flatfoot is one of the most common types of flatfoot. It typically begins in childhood or adolescence and continues into adulthood. It usually occurs in both feet and generally progresses in severity throughout the adult years. As the deformity worsens, the soft tissues (tendons and ligaments) of the arch may stretch or tear and can become inflamed.
The term "flexible" means that while the foot is flat when standing (weight-bearing), the arch returns when not standing. In the early stages of flexible flatfoot arthritis is not restricting motion of the arch and foot, but in the later stages arthritis may develop to such a point that the arch and foot become stiff.
Symptoms, which may occur in some persons with flexible flatfoot, include:
Shoe modifications. The foot and ankle surgeon will advise you on footwear characteristics that are important for the child with flatfoot.
When is Surgery Needed?
In some cases, surgery is necessary to relieve the symptoms and improve foot function. Foot and ankle sugeons perform a variety of techniques to treat the different types of pediatric flatfoot. The surgical procedure or combination of procedures selected for your child will depend on his or her particular type of flatfoot and degree of deformity.
Adult Flexible Flatfoot
Flexible flatfoot is one of the most common types of flatfoot. It typically begins in childhood or adolescence and continues into adulthood. It usually occurs in both feet and generally progresses in severity throughout the adult years. As the deformity worsens, the soft tissues (tendons and ligaments) of the arch may stretch or tear and can become inflamed.
The term "flexible" means that while the foot is flat when standing (weight-bearing), the arch returns when not standing. In the early stages of flexible flatfoot arthritis is not restricting motion of the arch and foot, but in the later stages arthritis may develop to such a point that the arch and foot become stiff.
Symptoms, which may occur in some persons with flexible flatfoot, include:
Pain in the heel, arch, ankle, or along the outside of the foot.
"Turned-in" ankle.
"Turned-in" ankle.
- Pain associated with a shin splint.
- General weakness/fatigue in the foot or leg
- Lumber back pain
Diagnosis of Flexible Flatfoot
In diagnosing flatfoot, you feet will be examined whilst sitting and standing, X-rays are usually taken to determine the severity of the disorder
Treatment Options
If you are diagnosed with flexible flatfoot, irrespective of whether you have symptoms, you will be advised of what you might expect in the future and various treatment options may be recommended, including:
In diagnosing flatfoot, you feet will be examined whilst sitting and standing, X-rays are usually taken to determine the severity of the disorder
Treatment Options
If you are diagnosed with flexible flatfoot, irrespective of whether you have symptoms, you will be advised of what you might expect in the future and various treatment options may be recommended, including:
- Activity modifications; cut down on activities that bring you pain and avoid prolonged walking and standing to give your arches a rest.
- Weight loss; if you are overweight, try to lose weight. Putting too much weight on your arches may aggravate your symptoms.
- Orthotic devices; custom orthotic devices can provided for your shoes to give more support to the arches.
- Immobilization; in some cases, it may be necessary to use a walking cast or to completely avoid weight-bearing.
- Medications; nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce pain and inflammation.
- Physical therapy; ultrasound therapy or other physical therapy modalities may be used to provide temporary relief.
- Shoe modifications; wearing shoes that support the arches is important for anyone who has flatfoot.
- HyProCure sinus tarsi implant; a minimally invasive (reversible) surgical procedure to correct hyperpronation of the foot.
- Surgery; in some patients whose pain is not adequately relieved by other treatments, surgery may be considered.
Flatfoot Surgery
A variety of surgical techniques are available to correct flexible flatfoot. Your case may require one procedure or a combination of procedures. All of these surgical techniques are aimed at relieving the symptoms and improving foot function. These procedures include the HyProCure sinus tarsi implant, tendon transfers or tendon lengthening procedures, realignment of one or more bones, joint fusions.
The procedure or combination of procedures that is used to correct flat foot deformity depends on many factors, including the cause and severity of the condition, as well as the patient's age, occupation and activity level. If surgery is performed, the length of the recovery period will vary, depending upon the procedure or procedures performed.
A variety of surgical techniques are available to correct flexible flatfoot. Your case may require one procedure or a combination of procedures. All of these surgical techniques are aimed at relieving the symptoms and improving foot function. These procedures include the HyProCure sinus tarsi implant, tendon transfers or tendon lengthening procedures, realignment of one or more bones, joint fusions.
The procedure or combination of procedures that is used to correct flat foot deformity depends on many factors, including the cause and severity of the condition, as well as the patient's age, occupation and activity level. If surgery is performed, the length of the recovery period will vary, depending upon the procedure or procedures performed.
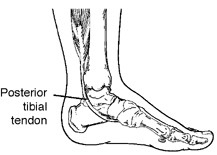
Adult Acquired Flatfoot
Posterior Tibial Tendon Dysfunction (PTTD)
What is PTTD?
Posterior Tibial Tendon Dysfunction (PTTD)
What is PTTD?
Posterior
tibial tendon dysfunction (PTTD) is an inflammation and/or
overstretching of the posterior tibial tendon in the foot. An important
function of the posterior tibial tendon is to help support the arch.
But in PTTD, the tendon’s ability to perform that job is impaired,
often resulting in a flattening of the foot.
The posterior tibial tendon is a fibrous cord that extends from a muscle in the leg. It descends the leg and runs along the inside of the ankle, down the side of the foot, and into the arch. This tendon serves as one of the major supporting structures of the foot and helps the foot to function while walking.
PTTD is often called “adult-acquired flatfoot” because it is the most common type of flatfoot developed during adulthood. Although this condition typically occurs in only one foot, some people may develop it in both feet. PTTD is usually progressive, which means it will keep getting worse—especially if it isn’t treated early.
Symptoms PTTD
The posterior tibial tendon is a fibrous cord that extends from a muscle in the leg. It descends the leg and runs along the inside of the ankle, down the side of the foot, and into the arch. This tendon serves as one of the major supporting structures of the foot and helps the foot to function while walking.
PTTD is often called “adult-acquired flatfoot” because it is the most common type of flatfoot developed during adulthood. Although this condition typically occurs in only one foot, some people may develop it in both feet. PTTD is usually progressive, which means it will keep getting worse—especially if it isn’t treated early.
Symptoms PTTD
The
symptoms of PTTD may include pain, swelling, a flattening of the arch,
and an inward rolling of the ankle. As the condition progresses, the
symptoms will change.
For example:
For example:
- When PTTD initially develops, typically there is pain on the inside of the foot and ankle (along the course of the tendon). In addition, the area may be red, warm, and swollen.
- Later, as the arch begins to flatten, there may still be pain on the inside of the foot and ankle. But at this point, the foot and toes begin to turn outward and the ankle rolls inward.
As PTTD becomes more advanced, the
arch flattens even more and the pain often shifts to the outside of the
foot, below the ankle. The tendon has deteriorated considerably and
arthritis often develops in the foot. In more severe cases, arthritis
may also develop in the ankle.
What Causes PTTD?
Overuse of the posterior tibial tendon is frequently the cause of PTTD which results from faulty function (biomechanics) associated with hyperpronation of the foot. In fact, the symptoms usually occur after activities that involve the tendon, such as running, walking, hiking, or climbing stairs.
Treatment: Non-surgical Approaches
Because of the progressive nature of PTTD, it is better to seek an opinion as soon as possible. If treated early enough, your symptoms may resolve without the need for surgery and progression of your condition can be arrested. In contrast, untreated PTTD could leave you with an extremely flat foot, painful arthritis in the foot and ankle, and increasing limitations on walking, running, or other activities.
In many cases of PTTD, treatment can begin with non-surgical approaches that may include:
What Causes PTTD?
Overuse of the posterior tibial tendon is frequently the cause of PTTD which results from faulty function (biomechanics) associated with hyperpronation of the foot. In fact, the symptoms usually occur after activities that involve the tendon, such as running, walking, hiking, or climbing stairs.
Treatment: Non-surgical Approaches
Because of the progressive nature of PTTD, it is better to seek an opinion as soon as possible. If treated early enough, your symptoms may resolve without the need for surgery and progression of your condition can be arrested. In contrast, untreated PTTD could leave you with an extremely flat foot, painful arthritis in the foot and ankle, and increasing limitations on walking, running, or other activities.
In many cases of PTTD, treatment can begin with non-surgical approaches that may include:
- Orthotic devices or bracing. To give your arch the support it needs, your foot and ankle surgeon may provide you with an ankle stirrup brace or a custom orthotic device that fits into the shoe.
- HyProCure sinus tarsi implant; a minimally invasive (reversible) surgical procedure to correct hyperpronation of the foot.
- Immobilization. Sometimes a short-leg cast or boot is worn to immobilize the foot and allow the tendon to heal, or you may need to completely avoid all weightbearing for a while.
- Physical therapy. Ultrasound therapy and exercises may help rehabilitate the tendon and muscle following immobilization.
- Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation.
- Shoe modifications. Your foot and ankle surgeon may advise you on changes to make with your shoes and may provide special inserts designed to improve arch support.
When is Surgery Needed?
In cases of PTTD that have progressed substantially or have failed to improve with non-surgical treatment, surgery may be required. For some advanced cases, surgery may be the only option. Surgical treatment may include repairing the tendon, realigning the bones of the foot, or both. If surgery is performed, the length of the recovery period will vary, depending upon the procedure or procedures performed.
In cases of PTTD that have progressed substantially or have failed to improve with non-surgical treatment, surgery may be required. For some advanced cases, surgery may be the only option. Surgical treatment may include repairing the tendon, realigning the bones of the foot, or both. If surgery is performed, the length of the recovery period will vary, depending upon the procedure or procedures performed.