Big Toe Joint Deformities
Bunions (Hallux Abductovalgus)
Even though bunions are a common foot deformity, there are misconceptions about them. Many people may unnecessarily suffer the pain of bunions for years before seeking treatment.
What is a Bunion?
Bunions (Hallux Abductovalgus)
Even though bunions are a common foot deformity, there are misconceptions about them. Many people may unnecessarily suffer the pain of bunions for years before seeking treatment.
What is a Bunion?
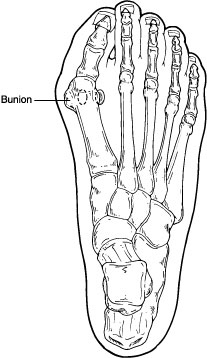
Bunions
are often described as a bump on the side of the big toe. But a bunion
is more than that. The visible bump actually reflects changes in the
bony framework of the front part of the foot. With a bunion, the big
toe leans toward the second toe, rather than pointing straight ahead.
This throws the bones out of alignment, producing the bunion's "bump."
Bunions
are a progressive disorder. They begin with a leaning of the big toe,
gradually changing the angle of the bones over the years and slowly
producing the characteristic bump, which continues to become
increasingly prominent. Usually the symptoms of bunions appear at later
stages, although some people never have symptoms.
What Causes a Bunion?
Bunions are most often caused by an inherited faulty mechanical structure of the foot. It is not the bunion itself that is inherited, but certain foot types that make a person prone to developing a bunion.
Although wearing shoes that crowd the toes won't actually cause bunions in the first place, it sometimes makes the deformity get progressively worse. That means you may experience symptoms sooner.
Symptoms
Symptoms occur most often when wearing shoes that crowd the toes—shoes with a tight toe box or high heels. This may explain why women are more likely to have symptoms than men. In addition, spending long periods of time on your feet can aggravate the symptoms of bunions.
Symptoms, which occur at the site of the bunion, may include:
Pain or soreness
Inflammation and redness
A burning sensation
Perhaps some numbness
Other conditions which may appear with bunions include calluses on the big toe, sores between the toes, ingrown toenail, and restricted motion of the toe.
Diagnosis
Bunions are readily apparent; you can see the prominence at the base of the big toe or side of the foot. However, to fully evaluate your condition, x-rays are required to determine the degree of the deformity and assess the changes that have occurred.
Because bunions are progressive, they don't go away, and will usually get worse over time. But not all cases are alike--some bunions progress more rapidly than others. Once your foot and ankle surgeon has evaluated your particular case, a treatment plan can be developed that is suited to your needs.
Treatment
Sometimes observation of the bunion is all that's needed. Periodic evaluation and x-ray examination can determine if your bunion deformity is advancing, thereby reducing your chance of irreversible damage to the joint. In many other cases, however, some type of treatment is needed.
Early treatments are aimed at easing the pain of bunions, but they won't reverse the deformity itself.
These options include:
Changes in footwear; wearing the right kind of shoes is very important. Choose shoes that have a wide toe box and forgo those with pointed toes or high heels which may aggravate the condition.
Padding; pads placed over the area of the bunion can help minimize pain. You can get bunion pads from your foot and ankle surgeon or purchase them at a drug store.
Bunions are most often caused by an inherited faulty mechanical structure of the foot. It is not the bunion itself that is inherited, but certain foot types that make a person prone to developing a bunion.
Although wearing shoes that crowd the toes won't actually cause bunions in the first place, it sometimes makes the deformity get progressively worse. That means you may experience symptoms sooner.
Symptoms
Symptoms occur most often when wearing shoes that crowd the toes—shoes with a tight toe box or high heels. This may explain why women are more likely to have symptoms than men. In addition, spending long periods of time on your feet can aggravate the symptoms of bunions.
Symptoms, which occur at the site of the bunion, may include:
Pain or soreness
Inflammation and redness
A burning sensation
Perhaps some numbness
Other conditions which may appear with bunions include calluses on the big toe, sores between the toes, ingrown toenail, and restricted motion of the toe.
Diagnosis
Bunions are readily apparent; you can see the prominence at the base of the big toe or side of the foot. However, to fully evaluate your condition, x-rays are required to determine the degree of the deformity and assess the changes that have occurred.
Because bunions are progressive, they don't go away, and will usually get worse over time. But not all cases are alike--some bunions progress more rapidly than others. Once your foot and ankle surgeon has evaluated your particular case, a treatment plan can be developed that is suited to your needs.
Treatment
Sometimes observation of the bunion is all that's needed. Periodic evaluation and x-ray examination can determine if your bunion deformity is advancing, thereby reducing your chance of irreversible damage to the joint. In many other cases, however, some type of treatment is needed.
Early treatments are aimed at easing the pain of bunions, but they won't reverse the deformity itself.
These options include:
Changes in footwear; wearing the right kind of shoes is very important. Choose shoes that have a wide toe box and forgo those with pointed toes or high heels which may aggravate the condition.
Padding; pads placed over the area of the bunion can help minimize pain. You can get bunion pads from your foot and ankle surgeon or purchase them at a drug store.
- Activity modifications; avoid activity that causes bunion pain, including standing for long periods of time.
- Medications; nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may help to relieve pain.
- Icing; applying an ice pack several times a day helps reduce inflammation and pain.
Injection
therapy; although rarely used in bunion treatment, injections of
corticosteroids may be useful in treating the inflamed bursa
(fluid-filled sac located in a joint) sometimes seen with bunions.
Orthotic devices; In some cases, custom orthotic devices may be helpful although difficulties often arise with altered fit of footwear.
HyProCure sinus tarsi implant; a minimally invasive (reversible) surgical procedure to correct hyperpronation of the foot.
When is Surgery Needed?
When the pain of a bunion interferes with daily activities, it's time to discuss surgical options to see if surgery is best for you.
Recent advances in surgical techniques have led to a very high success rate in treating bunions.
A variety of surgical procedures are performed to treat bunions. The procedures are designed to remove the "bump" of bone, correct the changes in the bony structure of the foot, as well as correct soft tissue changes that may also have occurred. The goal of these corrections is the elimination of pain.
The procedure that is used to correct the deformity depends on many factors, including the cause and extent of the deformity, x-ray findings, your age, occupation and activity level. If surgery is performed, the length of the recovery period will vary, depending upon the procedure or procedures performed.
Hallux Limitus & Rigidus
Hallux Rigidus
Each day, with every step you take, your big toe bears a tremendous amount of stress—a force equal to about twice your body weight. Most of us don't realize how much we use our big toe. We tend to take it for granted, unless a problem develops.
One problem that afflicts the big toe is called hallux rigidus, a condition where movement of the toe is restricted to varying degrees. This disorder can be very troubling and even disabling, since we use the all-important big toe whenever we walk, stoop down, climb up, or even stand. If you have pain and/or stiffness in your big toe, you may have this condition.
What is Hallux Rigidus?
Orthotic devices; In some cases, custom orthotic devices may be helpful although difficulties often arise with altered fit of footwear.
HyProCure sinus tarsi implant; a minimally invasive (reversible) surgical procedure to correct hyperpronation of the foot.
When is Surgery Needed?
When the pain of a bunion interferes with daily activities, it's time to discuss surgical options to see if surgery is best for you.
Recent advances in surgical techniques have led to a very high success rate in treating bunions.
A variety of surgical procedures are performed to treat bunions. The procedures are designed to remove the "bump" of bone, correct the changes in the bony structure of the foot, as well as correct soft tissue changes that may also have occurred. The goal of these corrections is the elimination of pain.
The procedure that is used to correct the deformity depends on many factors, including the cause and extent of the deformity, x-ray findings, your age, occupation and activity level. If surgery is performed, the length of the recovery period will vary, depending upon the procedure or procedures performed.
Hallux Limitus & Rigidus
Hallux Rigidus
Each day, with every step you take, your big toe bears a tremendous amount of stress—a force equal to about twice your body weight. Most of us don't realize how much we use our big toe. We tend to take it for granted, unless a problem develops.
One problem that afflicts the big toe is called hallux rigidus, a condition where movement of the toe is restricted to varying degrees. This disorder can be very troubling and even disabling, since we use the all-important big toe whenever we walk, stoop down, climb up, or even stand. If you have pain and/or stiffness in your big toe, you may have this condition.
What is Hallux Rigidus?
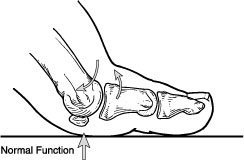
Hallux
rigidus is a disorder of the joint located at the base of the big toe.
It causes pain and stiffness in the big toe, and with time it gets
increasingly harder to bend the toe. "Hallux" refers to the big toe,
while "rigidus" indicates that the toe is rigid and cannot move. Hallux
rigidus is actually a form of degenerative arthritis (a wearing out of
the cartilage within the joint that occurs in the foot and other parts
of the body).
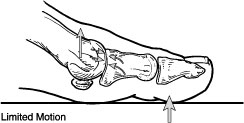
Because hallux rigidus is a progressive
condition, the toe's motion decreases as time goes on. In its earlier
stage, motion of the big toe is only somewhat limited—at that point,
the condition is called “hallux limitus.” But as the problem advances,
the toe's range of motion gradually decreases until it potentially
reaches the end stage of "rigidus"— where the big toe becomes stiff, or
what is sometimes called a "frozen joint." Other problems are also
likely to occur as the disorder progresses.
Early signs and symptoms include:
Pain and stiffness in the big toe during use (walking, standing, bending, etc.)
Pain and stiffness in the big toe during use (walking, standing, bending, etc.)
- Pain and stiffness aggravated by cold, damp weather
- Difficulty with certain activities (running, squatting)
As the disorder gets more serious, additional symptoms may develop, including:
- Swelling and inflammation around the joint
- Pain, even during rest
- Difficulty wearing shoes because bone spurs (overgrowths) develop. Wearing high-heeled shoes can be particularly difficult.
- Dull pain in the hip, knee, or lower back due to changes in the way you walk
- Limping, in severe cases
What Causes Hallux Rigidus?
Common
causes of hallux rigidus are faulty function (biomechanics) and
structural abnormalities of the foot that can lead to osteoarthritis in
the big toe joint. This type of arthritis—the kind that results from
"wear and tear"—often develops in people who have defects that change
the way their foot and big toe functions. For example, those
with fallen arches or excessive pronation (rolling in) of the ankles
are susceptible to developing hallux rigidus.
In some people,
hallux rigidus runs in the family and is a result of inheriting a foot
type that is prone to developing this condition. In other cases, it is
associated with overuse—especially among people engaged in activities
or jobs that increase the stress on the big toe, such as workers who
often have to stoop or squat. Hallux rigidus can also result from an
injury—even from stubbing your toe. Or it may be caused by certain
inflammatory diseases, such as rheumatoid arthritis or gout. Your foot
and ankle surgeon can determine the cause of your hallux rigidus and
recommend the best treatment.
Diagnosis of Hallux Rigidus
The sooner this condition is diagnosed, the easier it is to treat. Therefore, the best time to see a foot and ankle surgeon is when you first notice that your big toe feels stiff or hurts when you walk, stand, bend over, or squat. If you wait until bone spurs develop, your condition is likely to be more difficult to manage.
In diagnosing hallux rigidus, your feet will be examined and the joint manipulated to determine its range of motion. X-rays are usually required to evaluate how much arthritis is present as well as to assess any bone spurs or other abnormalities that may have formed.
Conservative Treatment
Treatment for mild or moderate cases of hallux rigidus may include one or more of the following:
The sooner this condition is diagnosed, the easier it is to treat. Therefore, the best time to see a foot and ankle surgeon is when you first notice that your big toe feels stiff or hurts when you walk, stand, bend over, or squat. If you wait until bone spurs develop, your condition is likely to be more difficult to manage.
In diagnosing hallux rigidus, your feet will be examined and the joint manipulated to determine its range of motion. X-rays are usually required to evaluate how much arthritis is present as well as to assess any bone spurs or other abnormalities that may have formed.
Conservative Treatment
Treatment for mild or moderate cases of hallux rigidus may include one or more of the following:
- Shoe modifications; shoes that have a large toe box should be worn, because they put less pressure on your toe. Stiff or rocker-bottom soles may also be recommended. Most likely, you will need to stop wearing high heels.
- Orthotic devices; custom orthotic devices may improve the function of your foot.
- Medications; nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be prescribed to help reduce pain and inflammation. Supplements such as glucosamine-chondroitin sulfate and some vitamins and minerals may also be helpful.
- Injection therapy; injections of corticosteroids in small amounts are sometimes given in the affected toe to help reduce the inflammation and pain.
- HyProCure sinus tarsi implant; a minimally invasive (reversible) surgical procedure to correct hyperpronation of the foot.
When is Surgery Needed?
In some cases, surgery is the only way to eliminate or reduce pain associated with the joint. There are several types of surgery that can be undertaken to treat hallux rigidus; these surgical procedures fall into two categories:
In some cases, surgery is the only way to eliminate or reduce pain associated with the joint. There are several types of surgery that can be undertaken to treat hallux rigidus; these surgical procedures fall into two categories:
- Some procedures reconstruct and "clean up" the joint removing the arthritic damage from the joint as well as any accompanying bone spurs, and then alter the position of one or more bones in the big toe. These procedures are designed to preserve and restore normal alignment and function of the joint as well as reduce or eliminate pain.
- More aggressive procedures are used when the joint cannot be preserved and may involve altering the position of one or more bones in the big toe in conjunction with implant arthroplasty, excisional arthroplasty or fusion of the joint.
The
procedure that is used to correct hallux rigidus depends on many
factors, including the cause of the condition and the severity, as well
as the patient's age, occupation and activity level. If surgery is
performed, the length of the recovery period will vary, depending upon
the procedure or procedures performed.